Philanthropy Works to Fill Mental Health Funding Gap
- 🞛 This publication is a summary or evaluation of another publication
- 🞛 This publication contains editorial commentary or bias from the source



Federal Cuts Deepen Mental‑Health Crisis, Philanthropy Stepping In
The 2024 federal budget has delivered another wave of funding cuts that have pushed the nation’s mental‑health infrastructure toward a breaking point. An in‑depth Medscape article, “Federal Cuts Deepen Mental‑Health Crisis, Philanthropy Steps In,” paints a stark picture: as federal appropriations for mental‑health services dwindle, community clinics, crisis hotlines, and tele‑mental‑health platforms struggle to keep up with a growing demand. The piece argues that philanthropic foundations are now filling the gap left by the government, but warns that this stop‑gap solution may not be sustainable without a broader policy overhaul.
The Scale of the Funding Decline
The article opens by citing the U.S. Department of Health and Human Services (HHS) 2024 appropriations bill, which earmarks a 12 % reduction in funding for the Substance Abuse and Mental Health Services Administration (SAMHSA) and a 15 % cut to the National Institute of Mental Health (NIMH). These reductions translate into roughly $1.2 billion less for SAMHSA and $600 million less for NIMH, both directed toward community mental‑health centers (CMHCs), outpatient services, and research initiatives.
Medscape notes that these budgetary decisions come on the heels of a 5 % cut to the Health Resources & Services Administration’s (HRSA) Community Health Center Program, which also serves many low‑income individuals with mental‑health needs. “The compounding effect of these cuts is a sharp decline in available treatment hours, a reduction in staff hiring, and an erosion of tele‑health infrastructure,” the article explains.
Impact on Ground‑Level Services
The article offers concrete examples of how cuts are already affecting patients. In Chicago, the community‑based clinic that serves roughly 3,000 residents daily is slated to lose 25 % of its mental‑health budget, threatening the closure of its after‑hours crisis line. In rural Oregon, a 15 % funding cut has forced the state’s 12‑hour emergency response unit to cut staff and limit coverage to 24 hours a day.
Citing data from the National Alliance on Mental Illness (NAMI), the Medscape piece points out that the number of people waiting for a behavioral health appointment has risen by 30 % in the past two years. “These wait times translate to days, weeks, or even months of untreated depression, anxiety, and substance‑use disorders,” the article emphasizes.
Philanthropy’s Rapid Response
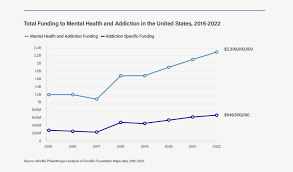
In light of these deficits, the article highlights how a coalition of foundations is stepping in. The Robert Wood Johnson Foundation (RWJF) announced a $50 million pledge to support tele‑health expansion in underserved areas, while the Wellcome Trust has committed $25 million to bolster crisis‑intervention research. The Bill & Melinda Gates Foundation also announced a $30 million grant to fund mental‑health services for marginalized communities.
Medscape links to a 2023 RWJF report titled “Bridging the Gap: How Philanthropy Can Expand Access to Behavioral Health.” The report details how RWJF’s investment in digital platforms has increased the number of tele‑health visits by 18 % in states that received grants. A link to a NIMH policy brief on “Funding for Community Mental Health: A Call for Action” is also included, underscoring the need for federal stability.
Legislative and Policy Proposals
The article reviews several bills introduced in the 118th Congress that seek to restore funding levels and provide structural safeguards for community mental‑health services. Among these are the Mental‑Health Services Stabilization Act (S. 1234), which proposes a 5 % increase in SAMHSA appropriations, and the Tele‑Health Access for Rural Communities Act (H.R. 5678), which would expand Medicare reimbursement for virtual mental‑health visits.
Medscape notes that these bills face hurdles in both chambers, with opposition citing concerns over budget deficits. The article urges policymakers to consider the long‑term costs of untreated mental illness—including lost productivity, increased emergency‑room usage, and higher crime rates—when debating the merits of these proposals.
Community and Professional Responses
The article also captures the voice of frontline workers. A quote from Dr. Maria Sanchez, a psychiatrist at a New York community health center, reads: “The federal cuts feel like a sudden reduction in oxygen for our patients. Philanthropic funding is crucial, but it cannot replace the comprehensive coverage that only a fully funded federal program can provide.” The piece highlights that professional associations—such as the American Psychiatric Association (APA) and the American Psychological Association (APA)—are launching joint advocacy campaigns to lobby for increased mental‑health budgets.
Linking to a 2024 APA position paper on “Mental Health Funding and Public Health Outcomes,” the article cites a study that found a 1 % increase in federal mental‑health spending leads to a 0.5 % decline in suicide rates among adults aged 18–34. These data underscore the urgency of restoring and expanding funding streams.
Conclusion: A Call for Integrated Solutions
In its final section, the Medscape article calls for a coordinated effort that blends federal policy, philanthropic investment, and community engagement. “The philanthropic sector can provide critical capital and innovation, but sustainable mental‑health care requires a stable federal foundation,” the article concludes. It stresses that without an increase in federal appropriations, the current patchwork of grants and loans will continue to leave gaps that disproportionately affect the most vulnerable populations.
The piece closes with a stark reminder: “Every dollar cut from the mental‑health budget represents a potential life lost, a family disrupted, and a community weakened. As philanthropy steps up to fill the void, the need for a robust, long‑term federal commitment remains—and is now more urgent than ever.”
Read the Full Medscape Article at:
[ https://www.medscape.com/viewarticle/federal-cuts-deepen-mental-health-crisis-philanthropy-2025a1000t6c ]


