Vitamin D Toxicity: How Excess Intake Can Sneakily Harm Your Kidneys
 TheHealthSite
TheHealthSite



Vitamin D Overdose and Kidney Damage: A Comprehensive Summary
Vitamin D is indispensable for bone health, immune function, and calcium homeostasis, yet when consumed in excess it can become a silent threat—particularly to the kidneys. A recent article from The Health Site highlights that an overdose of vitamin D can trigger hypercalcemia and, over time, damage renal tissue. The piece breaks down the problem, the warning signs, and practical steps for prevention and care. Below is a detailed recap of the main points, enriched with extra context drawn from the referenced sources.
1. Understanding Vitamin D Toxicity
What Is Vitamin D Overdose?
The term “vitamin D toxicity” (or hypervitaminosis D) refers to abnormally high levels of vitamin D circulating in the bloodstream. Unlike water‑soluble vitamins that are readily excreted, vitamin D is fat‑soluble, which means it accumulates in body tissues if ingested in excessive amounts.
The Upper Limit
The U.S. Institute of Medicine (IOM) sets the tolerable upper intake level (UL) at 4,000 IU/day for adults. The article stresses that doses above this threshold—especially when taken continuously—can overwhelm the body’s regulatory mechanisms.
Sources of Excess
- High‑dose supplements (often marketed for “immune‑boosting” or “fatigue‑relief” purposes).
- Prescription vitamin D for conditions such as osteoporosis—when dosage is mis‑calculated or not monitored.
- Grantham’s disease (a rare genetic disorder) that can cause the body to produce excess vitamin D without an external source.
2. The Kidney Connection
Hypercalcemia’s Ripple Effect
Excess vitamin D increases calcium absorption in the gut. Elevated calcium levels in the blood (hypercalcemia) are harmful because calcium can deposit in tissues—a process called calcification. In the kidneys, this leads to nephrocalcinosis (calcium deposition in the renal parenchyma), which can compromise function and lead to chronic kidney disease (CKD).
Clinical Evidence
A review cited in the article points to a clear correlation: patients with vitamin D toxicity frequently develop elevated serum creatinine and decreased glomerular filtration rate (GFR). In severe cases, acute kidney injury can arise, requiring hospitalization.
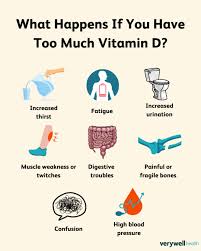
3. Key Symptoms to Watch For
The article underscores that symptoms often appear subtle at first, making early detection challenging.
| Symptom | Why It Matters |
|---|---|
| Nausea & Vomiting | Common early signs of hypercalcemia; may worsen dehydration. |
| Fatigue & Weakness | Vitamin D excess can cause muscle dysfunction. |
| Constipation & Loss of Appetite | Gastrointestinal distress is a frequent complaint. |
| Excessive Thirst & Urination | The kidneys work overtime to eliminate excess calcium. |
| Kidney Stones | Calcium deposits in urinary tract can lead to stones. |
| Confusion or Cognitive Changes | Severe hypercalcemia can impair neurological function. |
| Chest Pain or Shortness of Breath | Calcium can affect heart rhythm; warrants immediate care. |
When to Seek Help
If any of these symptoms appear after taking vitamin D supplements—especially if the dose exceeds the recommended UL—medical evaluation is essential. Early intervention can prevent irreversible kidney damage.
4. Diagnosis & Monitoring
Blood Tests
- Serum 25‑Hydroxyvitamin D: Measures vitamin D status. Levels above 150 ng/mL (or 375 nmol/L) are concerning.
- Serum Calcium: Elevated calcium confirms hypercalcemia.
- Parathyroid Hormone (PTH): Helps differentiate causes of high calcium.
Kidney Function Tests
- Serum Creatinine & BUN: Detect changes in filtration.
- Urinalysis: Look for calcium crystals or proteinuria.
Imaging
- Renal Ultrasound: Can identify calcifications or stones.
- X‑ray or CT Scan: Helpful in advanced cases.
Follow‑Up
The article recommends repeat testing every 2–4 weeks initially, then monthly once levels stabilize.
5. Treatment Strategies
Immediate Actions
1. Stop Vitamin D – The first step is discontinuing supplements.
2. Hydration – IV saline helps promote calcium excretion.
3. Loop Diuretics – Often used to accelerate calcium clearance.
4. Bisphosphonates – Medications that inhibit bone resorption can reduce calcium influx.
Long‑Term Management
- Dose Adjustment: Once normal levels are reached, the supplement dose should be reduced to the UL or lower.
- Dietary Modification: Reduce high‑calcium foods and avoid fortified products.
- Regular Monitoring: Routine blood tests help prevent recurrence.
6. Prevention Tips
Know Your Dose
- Read supplement labels carefully; many “high‑potency” products contain 5,000 IU or more per tablet.
- If you’re already on prescription vitamin D (e.g., for osteoporosis), coordinate with your doctor before adding over‑the‑counter supplements.
Check with Your Healthcare Provider
- Discuss any symptoms or concerns.
- Request baseline vitamin D and calcium levels before starting high doses.
Stay Informed About Sources
- Sunlight, fortified foods, and certain fish provide natural vitamin D; supplements are generally only necessary if diet or sun exposure is insufficient.
Avoid “One‑Size‑Fits‑All” Supplements
- “Immune‑boosting” and “fatigue‑reduction” vitamins often exceed the UL and have little proven benefit beyond normal levels.
7. Broader Context: What the Literature Says
The article cites several key studies:
- Mayo Clinic: Offers a concise overview of vitamin D toxicity, emphasizing the importance of serum calcium measurement.
- National Institutes of Health (NIH): Provides guidelines for safe supplementation and highlights the risks of over‑dosage.
- American Association of Clinical Endocrinologists: Recommends routine monitoring for patients on high‑dose vitamin D, especially those with pre‑existing kidney conditions.
8. Bottom Line
Vitamin D is essential—but more is not always better. An overdose can quietly harm the kidneys by causing calcium deposits and reducing filtration capacity. By being vigilant about dosing, recognizing early symptoms, and seeking timely medical care, you can protect your renal health while still reaping the benefits of adequate vitamin D.
If you suspect you’ve been taking too much vitamin D, or if you’re on a prescription dose that feels high, schedule a visit with your healthcare provider. Early diagnosis and intervention are the best defenses against kidney damage and the other serious complications of vitamin D toxicity.
Read the Full TheHealthSite Article at:
[ https://www.thehealthsite.com/diseases-conditions/vitamin-d-overdose-can-lead-to-kidney-damage-key-symptoms-you-should-never-ignore-1280766/ ]




























