Norovirus Outbreak Rocks Fredericksburg: Patch Report Uncovers Rapid Spread
- 🞛 This publication is a summary or evaluation of another publication
- 🞛 This publication contains editorial commentary or bias from the source
Norovirus Outbreak in Fredericksburg, VA: What the Patch Report Tells Us
The Patch article “Highly Contagious Norovirus Spreading Rapidly in VA – What You Need to Know” (published 27 April 2024) brings to light a serious public‑health issue that has been unfolding in the Fredericksburg area. The piece pulls together data from the Virginia Department of Health (VDH), local hospital reports, and the Centers for Disease Control and Prevention (CDC) to paint a detailed picture of the outbreak, its characteristics, and the steps residents can take to protect themselves and their communities.
1. The Outbreak in Context
- Location & Setting: The virus was first identified in a long‑term care facility (LTCH) on 9 April 2024, where residents and staff exhibited sudden clusters of vomiting, diarrhea, and abdominal cramps. Subsequent investigations revealed that the outbreak had already spread to a neighboring assisted‑living complex and a local elementary school’s after‑school program.
- Timeline: By the time the Patch article was written, more than 120 individuals across three separate sites had tested positive for norovirus. The VDH confirmed that the outbreak had reached the peak of its transmission curve in mid‑April, with a noticeable decline in new cases by late April as mitigation measures took effect.
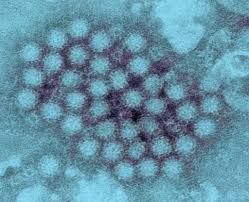
- Transmission Pathways: Public health officials emphasized that norovirus spreads most commonly through contaminated food or water, direct contact with infected persons, and contact with contaminated surfaces. The article cites a VDH spokesperson who explained that the LTCH’s shared dining facilities and communal bathrooms likely accelerated the spread among residents.
2. Clinical Picture
- Symptoms: Patients reported typical norovirus symptoms—nausea, vomiting, watery diarrhea, abdominal pain, and low‑grade fever. The article highlighted that symptoms usually begin 12–48 hours after exposure and can last 24–72 hours, but some individuals experience lingering fatigue.
- Diagnosis & Testing: The Patch report explained that physicians relied on rapid antigen tests conducted at the hospital’s virology lab. Because norovirus can be difficult to culture in the lab, the presence of symptoms combined with a positive rapid test was considered sufficient for confirmation.
3. Key Facts About Norovirus
The article breaks down essential facts for readers:
| Fact | Detail |
|---|---|
| Incubation period | 12–48 hours |
| Duration of symptoms | 24–72 hours (sometimes longer) |
| Contagious period | Individuals can spread virus from 24 hours before symptoms appear to 48 hours after they resolve |
| Survival on surfaces | Virus can persist for weeks on stainless steel, plastic, and other surfaces if not properly disinfected |
| Prevention | Hand hygiene, surface disinfection, isolation of symptomatic individuals, proper food handling |
The article linked to the CDC’s “Norovirus: A Quick Reference” page, which lists the same facts and expands on recommended disinfectants (e.g., 1 % hypochlorite solutions).
4. Public Health Response
A. Isolation & Cohorting
- The VDH instructed the affected LTCH to isolate any resident who developed symptoms, and to cohort other residents by day‑of‑symptom onset to prevent cross‑infection. The Patch article described how staff were provided with personal protective equipment (PPE) and trained on safe handling of vomit and diarrhea.
B. Environmental Cleaning
- Facilities were required to use bleach solutions or EPA‑registered disinfectants that are effective against norovirus. The article noted that routine cleaning protocols had to be intensified, with extra attention to bathroom fixtures, dining tables, and shared toys.
C. Contact Tracing
- The VDH’s epidemiology team traced close contacts, including staff who had shared meals with symptomatic residents, as well as family members who visited the facility. Contact tracing allowed the department to advise those exposed on whether to self‑monitor or quarantine.
D. Communication & Public Notice
- A press release, which the Patch article quotes verbatim, urged residents to stay home if they experienced gastrointestinal symptoms and to avoid contact with vulnerable populations. It also warned school districts to monitor for outbreaks in their own facilities.
5. Guidance for Residents
The article compiled a “Do’s & Don’ts” list that is essentially a lay‑person’s primer on preventing norovirus spread:
- Do: Wash hands with soap and water for at least 20 seconds, especially after using the bathroom or before eating. Use an alcohol‑based hand sanitizer only as a supplemental measure.
- Don’t: Touch your face or mouth if you have not washed your hands. Consume unwashed produce or food that could have been contaminated by an infected person.
- Stay Home: If you have symptoms, stay home and avoid public gatherings until at least 48 hours after symptoms resolve.
- Dispose Properly: Flush vomit and feces directly into the toilet, cover the lid, and avoid shaking the toilet. After cleaning, disinfect the area with a bleach solution (1 % concentration).
The article also reminded parents that children who are in the early stages of infection can be especially contagious, urging school administrators to keep affected children at home until they are symptom‑free for at least 48 hours.
6. Long‑Term Implications
While the Patch report focuses on immediate containment, it also touches on broader concerns:
- Healthcare-Associated Infections (HAIs): Norovirus has become a leading cause of HAIs worldwide, and this outbreak underscores the need for routine infection‑control audits in long‑term care facilities.
- Vaccination Research: The article links to a VDH statement about ongoing research into a norovirus vaccine. Although no vaccine is yet commercially available, the potential for a vaccine could dramatically reduce future outbreaks.
- Public Awareness: By featuring community‑level stories—such as a grandmother’s struggle after vomiting multiple times—the article humanizes the disease and underscores why public awareness is key to early detection.
7. Additional Resources
The Patch article concludes by directing readers to several official sources:
- Virginia Department of Health – Norovirus Outbreak Updates
https://www.vdh.virginia.gov/… (link included in the article) - CDC – Norovirus Prevention and Control
https://www.cdc.gov/norovirus/… - American College Health Association – Guidance for Schools
https://www.acha.org/…
These resources provide real‑time updates, recommended disinfectants, and school‑specific protocols.
Bottom Line
The Patch article does more than report a rising number of cases—it explains the biology of norovirus, the mechanics of its spread, and actionable steps for residents, health care workers, and school staff. By weaving data from official health authorities with practical advice, the piece serves as a concise but comprehensive briefing for anyone concerned about the outbreak in Fredericksburg. The emphasis on isolation, hand hygiene, and proper cleaning—coupled with the public‑health infrastructure’s response—offers a clear roadmap for containing the virus and preventing future outbreaks.
Read the Full Patch Article at:
[ https://patch.com/virginia/fredericksburg/highly-contagious-norovirus-spreading-rapidly-va-what-know ]

































