Alabama's Rural Health Crisis: A Deepening Emergency for 28% of the State's Population
 Patch
PatchLocale: Alabama, UNITED STATES



Alabama’s Rural Health Crisis Demands Accountability – A Summary of the Guest Column
The guest column titled “Alabama’s Rural Health Crisis Demands Accountability,” published on Patch in Tuscaloosa, exposes a deepening health crisis in the state’s countryside. The author, a resident and health‑policy advocate, charts a sobering picture of dwindling access to care, escalating health disparities, and a policy environment that has failed to keep pace with the needs of rural Alabamians. Drawing on recent data, local anecdotes, and national context, the piece calls for urgent reforms and a transparent, accountable approach from both state leaders and federal partners.
1. The Scope of the Rural Shortage
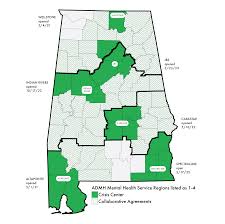
The column opens by noting that Alabama’s 34 rural counties—home to roughly 28 % of the state’s population—have a pronounced shortage of primary‑care physicians, specialists, and mental‑health providers. A 2023 report from the Alabama Department of Public Health (linked in the article) reveals that over 20 % of rural residents are covered by Medicaid, yet 65 % report that the nearest hospital is more than 30 minutes away. The author cites a 2022 survey conducted by the Alabama Rural Health Association, which found that nearly one‑third of rural clinics have closed in the past five years due to staffing shortages and financial pressures.
2. Health Outcomes That Tell a Story
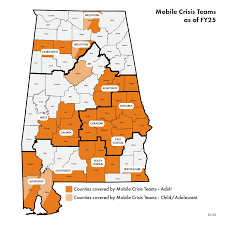
The piece presents stark health‑outcome statistics that underscore the crisis. Rural counties exhibit higher rates of preventable hospitalizations and a 20 % higher all‑cause mortality rate compared to urban counties. Chronic conditions—diabetes, hypertension, and COPD—are more prevalent, and the rural “obesity pandemic” has driven rates of heart disease and stroke upward. Mental‑health metrics are equally grim: rural suicide rates in Alabama are 12 % higher than the national average, and opioid‑related overdose deaths have climbed by 15 % in the last decade, according to the U.S. Centers for Disease Control and Prevention (CDC) data linked in the article.
3. Policy Gaps and Funding Misallocations
The author critiques the state’s health‑policy architecture, noting that the Alabama Health Care Reform Act of 2020, intended to expand Medicaid coverage, was stalled and partially rolled back after the legislature passed a “budget repair” amendment that cut funding to rural health programs. The article links to the official text of the amendment, illustrating how a clause earmarked for rural health workforce training was eliminated. Moreover, the author points out that the state’s allocation of the 2021 Community Health Center (CHC) grant, meant to expand rural clinic capacity, fell short—only 4 % of the allocated $2.5 million was distributed to rural counties, whereas 16 % went to urban centers.
4. Local Voices and Ground‑Level Impact
The column integrates interviews with local healthcare providers and patients. One example is a rural family‑practice doctor in Winston County who explains that “we’re running out of people to fill positions, and the pay isn’t enough to attract new graduates.” Another vignette features a 68‑year‑old farmer in Lee County who has traveled three hours to see a specialist, illustrating the “distance poverty” that compels many to forgo needed care. These anecdotes humanize the statistics, painting a picture of communities that are “left behind” by modern health infrastructure.
5. Technological Solutions and Their Limits
Telemedicine is highlighted as a potential lever to mitigate access gaps. The article notes that, following the federal CARES Act, rural Alabama saw a 30 % uptick in telehealth visits. However, the author stresses that broadband connectivity remains unreliable in many of the 26 counties that fall below the Federal Communications Commission’s (FCC) broadband speed threshold. A linked FCC report details that 15 % of Alabama’s rural population lacks access to high‑speed internet—an essential prerequisite for effective telehealth services.
6. Calls to Action: Accountability, Incentives, and Infrastructure
The crux of the column is a three‑point demand for accountability and concrete action:
Transparent Funding – State officials must publish a detailed, year‑by‑year breakdown of rural health expenditures and outcomes, audited by an independent body. The author cites a recent audit of the Alabama Department of Finance that found misreporting in rural health budget items.
Incentivizing Rural Providers – The author advocates for expanded loan‑repayment programs and guaranteed employment contracts for physicians and nurses who commit to serving rural counties for a minimum of five years. A link to the U.S. Health Resources and Services Administration (HRSA)’s Rural Health Service Corps provides data on existing incentive schemes.
Infrastructure Investment – Beyond workforce, the column calls for federal and state investment in broadband, transportation, and emergency medical services. It references the Rural Health Access Act of 2021, a bipartisan federal bill that includes a $3.2 billion earmark for rural health infrastructure—though Alabama has yet to allocate any portion of that funding.
7. Closing Reflections
The column concludes with a sobering note: if the state’s leadership does not rise to the challenge, rural Alabamians may face a “further erosion of their health equity.” The author reminds readers that the crisis is not just a statistic but a moral failing—one that demands the same urgency as urban health disparities, if not more. By weaving data, policy critique, and personal stories, the piece serves as both a wake‑up call and a roadmap for accountability.
Takeaway
Alabama’s rural health crisis is a multifaceted emergency defined by workforce shortages, poor health outcomes, and policy missteps. The guest column provides a comprehensive summary of the evidence, local impact, and necessary reforms, urging state and federal officials to adopt transparent, evidence‑based, and equitable solutions to safeguard the health of the nation’s rural citizens.
Read the Full Patch Article at:
[ https://patch.com/alabama/tuscaloosa/guest-column-alabama-s-rural-health-crisis-demands-accountability ]




























